Transforming Lives Through Leading-Edge Brain Aneurysm and AVM Research
Looking back on our high school years, we might remember the teachers we liked, cheering at football games, and chatting with friends in the hallway between classes. The things that made high school fun.
Joey Jean Farmer’s high school memories include all those things, yet also something entirely different.
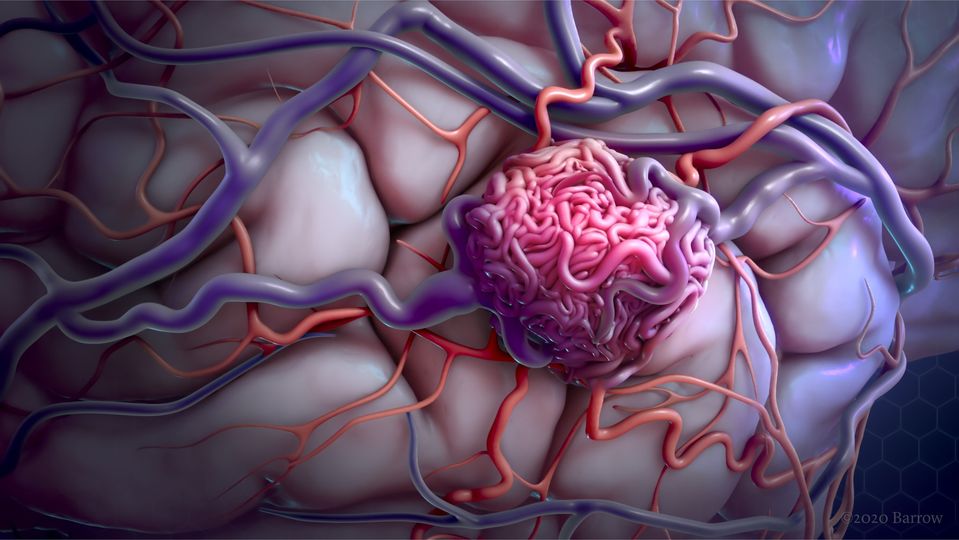
At 14, Joey Jean experienced a severe migraine attack, during which her entire left side went numb. An MRI revealed an arteriovenous malformation (AVM), an abnormal tangle of weak and poorly formed blood vessels. Her AVM was intracranial—located inside her brain. An AVM can rupture at any time, causing intense bleeding and a stroke that may lead to severe disability or death.
“I’ll never forget the day my dad explained to me that I had a Grade 5 AVM, which is considered inoperable, or how my mom cried and hugged me afterward,” Joey Jean says. The doctors they consulted told them that the AVM was inoperable due to its large size and its location near the brain’s occipital lobe, which contains the visual cortex. All they could do was treat Joey Jean’s symptoms.
Well, the Farmer family wasn’t going to settle for that. Eventually, they found a surgeon who could offer them a solution: Michael T. Lawton, MD, President and CEO of Barrow Neurological Institute and founder and director of the Barrow Aneurysm and AVM Research Center (BAARC). As one of the most experienced clinicians in this field, Dr. Lawton has treated more than 1,200 AVMs, as well as more than 5,250 aneurysms.
Before: A Very Precarious Position
Few neurological conditions are as complex and potentially life-threatening as aneurysms and AVMs. An aneurysm is an outward bulging, like a bubble or balloon, caused by a weak spot on a blood vessel wall. Approximately 300,000 Americans have AVMs of the brain or spinal cord, and one cerebral (brain) aneurysm ruptures every 18 minutes.
According to the National Institute of Neurological Disorders and Stroke (NINDS), most AVMs are present at birth, and others develop during a person’s first 20 years of age. Some make their presence known through seizures or headaches, but more often, people don’t even know they have one—a dangerous hemorrhage might be the first and only clue. More than 50% of AVM ruptures are fatal. Those who survive a rupture usually are left with permanent, life-altering neurological deficits, similar to a severe stroke. Experiencing a sudden, incredibly painful headache—more severe than any headache, ever—is a signal that you should seek emergency care immediately.
Today, however, it is more common to detect an AVM before it ruptures. Advances in magnetic resonance imaging (MRI) and computed tomography (CT) for neuroimaging have made it easier to detect AVMs and visualize their extent faster and more accurately than was possible in the past.
Deciding how best to treat an AVM, particularly one in the brain, presents a quandary. Options include resection (surgical removal, which is curative), embolization to block off the abnormal vessels and reduce the risk of rupture, and Gamma Knife radiotherapy to shrink the AVM and close off the vessels over time. In some cases, operating on an AVM can lead to severe complications for the patient. The key is to determine which patients will benefit from surgery and which ones are at risk for experiencing adverse effects. Also, while in the past these treatment options were considered on an either/or basis, today they often are used together to provide the optimal outcome for the patient.
Evaluating specific characteristics of a particular AVM can help neurosurgeons predict the most likely surgical outcome. In 1986, Robert Spetzler, MD, who was President and CEO of Barrow until his retirement in 2017, co-created the Spetzler-Martin AVM Grading Scale to classify AVMs based on their size, location in the brain, and clinical characteristics, giving them a score of 1 to 5. The higher the grade, the greater the risk of complications. This grading scale revolutionized how AVMs are approached clinically, providing a standardized framework for assessing their severity and guiding treatment decisions. It is the most commonly used AVM grading system by neurosurgeons worldwide. In 2010, Dr. Lawton refined the classification with additional variables, making it even more useful than before.
In Joey Jean’s case, her Grade 5 AVM was inoperable, so Dr. Lawton proposed that she undergo Gamma Knife radiotherapy to shrink it until it reached an operable state. She agreed to the treatment plan, but it wasn’t easy. She says, “While my friends were doing sports and planning for college, I was dealing with migraine attacks, medications, and radiation therapy.”
Joey Jean finished all of her treatments before starting her senior year of high school, “which excited me beyond belief!” she says. Her AVM was not yet removed, but it would be carefully monitored.
After: A New Lease on Life
After her radiotherapy treatments, Joey Jean enjoyed her senior year of high school, spending time with her friends and getting ready for college. But that wasn’t the end of her story.
“One year later, I was sitting in a college lecture when pain like I’d never experienced before sliced through my head. When I got [to the hospital], I found out that my AVM had ruptured and I had suffered a stroke,” she recalls.
There was no time left to wait. Her AVM needed to be removed, immediately. But the surgery was going to be risky. She says, “There was only one surgeon in the world I trusted to perform the operation: Dr. Lawton.”
On May 23, 2019, the day Joey Jean had been fearing for years finally came. Her surgery went well, but another part of the AVM was still hidden behind some tissue. “That meant I had to go in for a second surgery to remove the rest of it. I was lucky I had made it through this one, and now I had to do it all over again in less than 12 hours. I was terrified that I’d wake up blind, or that I wouldn’t wake up at all.”
Recovery from AVM interventions varies depending on the size and location of the malformation, as well as the chosen treatment. Physical therapy and rehabilitation help patients regain lost function and adjust to any residual neurological deficits. Joey Jean’s surgery was successful, and thankfully, she woke up with no major neurological deficits. But she still had a lot of healing ahead of her.
“I don’t know how I would have made it through those first few days without the kindness and compassion of the Barrow Neuro-ICU nurses,” she says. One nurse in particular, Virginia Prendergast, PhD, NP-C, FAAN, had a life-changing impact on her. “We talked about my desire to go to nursing school, and she validated that nursing was the career path for me,” says Joey Jean. “On my last day at Barrow, we made a pact that I would come back one day and share my story.”
In October 2022, she did just that, speaking at the Barrow Neuroscience Nursing Symposium. Joey Jean had graduated from nursing school and was on her way to achieving her dream: becoming a pediatric ICU nurse, “helping other children just like my nurses helped me.”
How Barrow Neurological Foundation Supports AVM Research
While saving the lives of patients like Joey Jean Farmer, Barrow Neurological Institute is also at the forefront of AVM and aneurysm research, serving as an international hub for interdisciplinary collaboration, fostering innovation, and pushing boundaries in the field. Researchers in the Barrow Aneurysm and AVM Research Center, like S. Paul Oh, PhD, are investigating the underlying genetics, formation, and rupture of aneurysms and AVMs to discover better ways to detect and treat them.
Donors who provide funding through Barrow Neurological Foundation play a vital role in fueling these research efforts, enabling Barrow Neurological Institute to conduct groundbreaking studies and invest in cutting-edge technologies.
The Foundation is funding several AVM research studies. In one, Dr. Oh has been working with the KRAS gene, which is linked to the formation of AVMs. When the KRAS gene is inhibited, the size of an AVM can be reduced; conversely, if you stop the inhibitor, KRAS is overexpressed, and the AVM will grow again. This important finding could lead to the development of a medication-based approach to stabilizing AVMs and preventing their rupture.
Dr. Oh has also begun using a new, Foundation-funded piece of equipment, the Iconeus One imaging system, to complement traditional MRI methods in studying brain AVMs. This high-powered ultrasound machine can monitor the presence, progression, and rupture of AVMs in preclinical models, which will be extremely beneficial to Dr. Oh and his team.
From earlier detection to innovative treatment modalities and ongoing research, Barrow continues to offer hope and improved outcomes for patients like Joey Jean Farmer and their families.
Funding for Aneurysm & AVM Research and Treatment
The Barrow Aneurysm and AVM Research Center is working continually to develop new, less invasive, and more effective treatments for aneurysms and AVMs. You can help. Support AVM and aneurysm research today by making a donation at SupportBarrow.org.
Donate to Aneurysm and AVM Research and Treatment Center at Barrow
When you support the world’s leading brain and spine specialists, you’re giving the tools necessary to provide the highest quality of care today while researching the cures for tomorrow. Help give more patients like Joey Jean Farmer the chance to live long, fulfilling lives with your donation today. Call us at (602) 406-3041 or visit us online.